Are you tired of spending more time on data entry than on actual billing?
Medical billing often feels like it’s all about typing and paperwork, with only a small fraction dedicated to handling the billing itself.
But here’s the good news: automation is changing the game!
By automating your billing and reimbursement processes, you can save time, cut costs, and streamline operations.
Automation simplifies those complex tasks, freeing you up to focus on what really matters—patient care.
Consider this: the average cost of reworking a single denied claim is $25, but when you multiply that by the number of claims, it adds up quickly.
In fact, correcting just 15 denied claims each month can cost your practice $4,500 a year, and denial rates can hit 5-15% or more.
Automation can boost your billing capacity by up to 250%, making the process faster and stress-free.
What Is Medical Billing Automation?
Medical billing automation is a smart solution that simplifies the entire billing process for healthcare providers.
It automates the gathering, creating, and submitting of bills to insurance companies and patients using technologies like robotic process automation (RPA), machine learning (ML), and artificial intelligence (AI).
By removing manual, repetitive tasks, automation makes billing faster, more accurate, and less prone to errors.
This not only improves revenue cycle management but also reduces the chances of claim delays or denials, which can frustrate patients.
In the end, it helps healthcare providers focus on care, not paperwork.
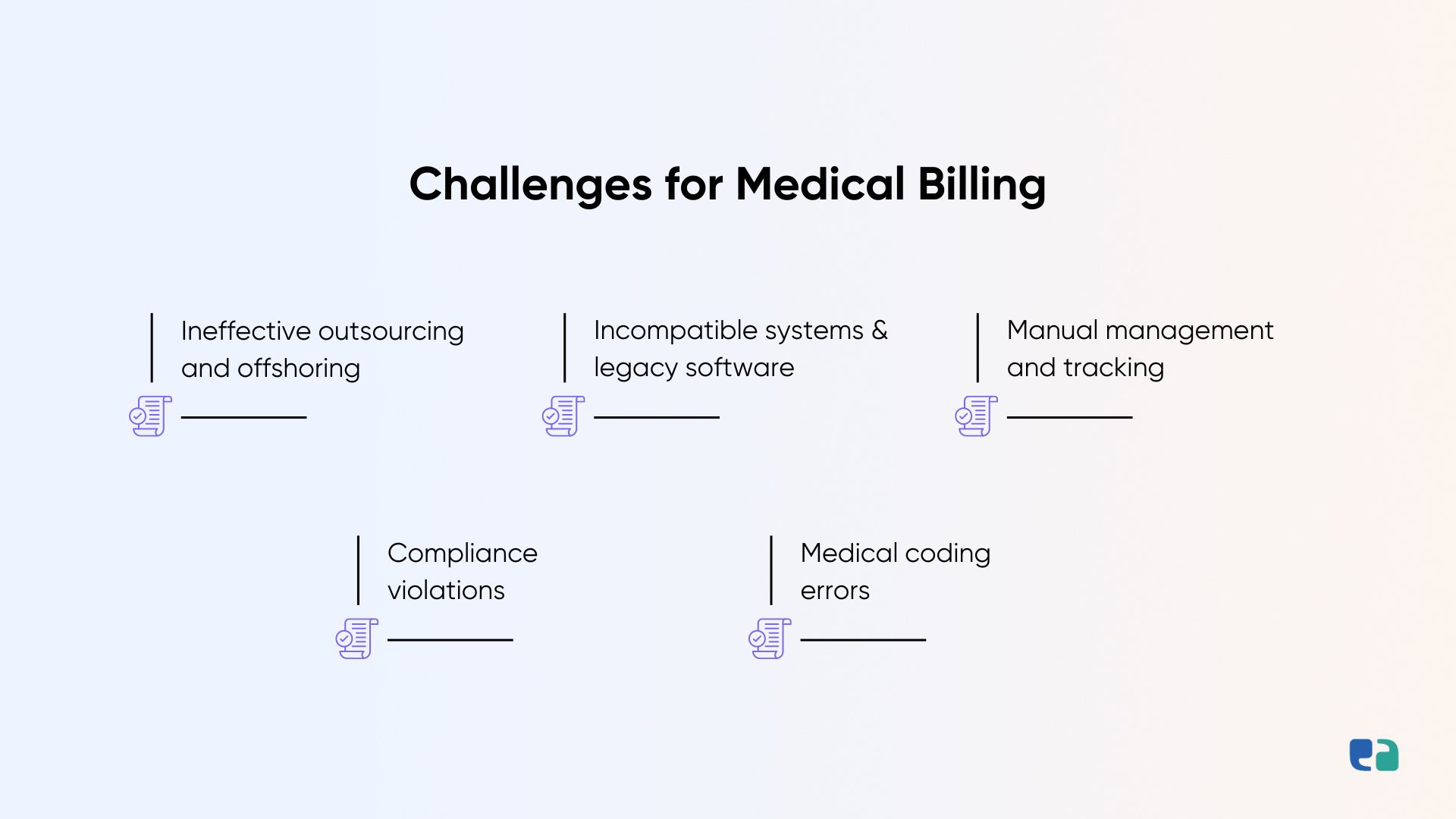
Why Does the Medical Billing System Need Automation?
Medical billing is full of inefficiencies. Here’s how automation can help:
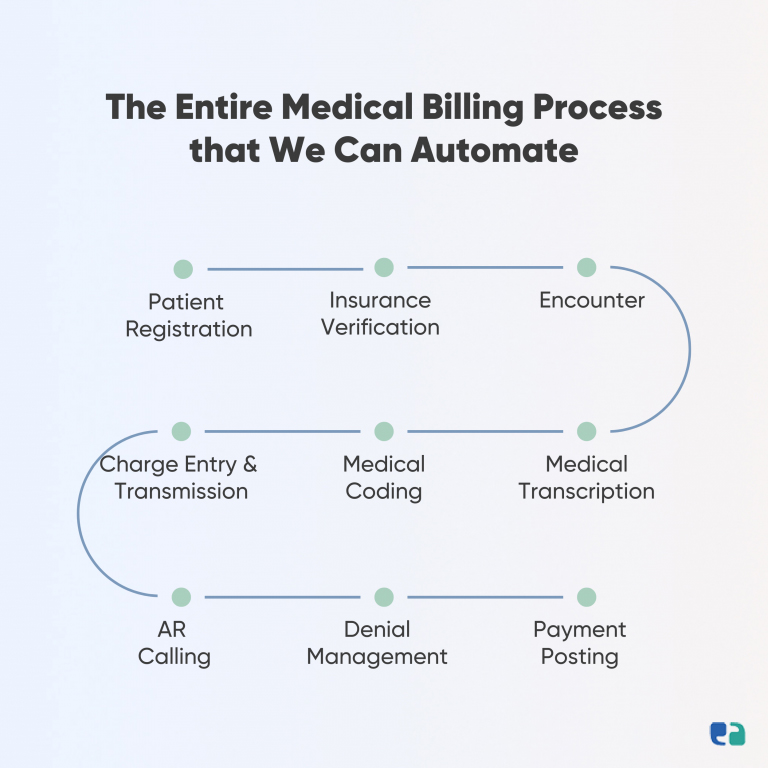
Key Processes to Automate in Medical Billing Systems
Looking to make your billing process smoother? Here are some key tasks you can automate:
- Patient Registration: Quickly capture and manage patient info.
- Claim Generation: Automatically create claims for billing.
- Insurance Verification: Check insurance coverage and eligibility with ease.
- Pre-authorizations: Handle authorization requests efficiently.
- Medical Coding: Ensure accurate coding for services.
- Claim Submission: Send claims to insurers without manual input.
- Claims Processing: Automate the review and processing of claims.
- Patient Statements: Prepare and follow up on patient bills.
- Payment Reconciliation: Match payments with claims automatically.
- Denial Management: Track and address claim denials swiftly.
- Reporting: Generate detailed reports effortlessly.
- Compliance Monitoring: Ensure adherence to regulations.
- Document Management: Organize and retrieve documents efficiently.
Real-Life Success Stories: The Power of Healthcare Automation
Let’s dive into how automation can truly transform your billing system with a couple of real-world examples.
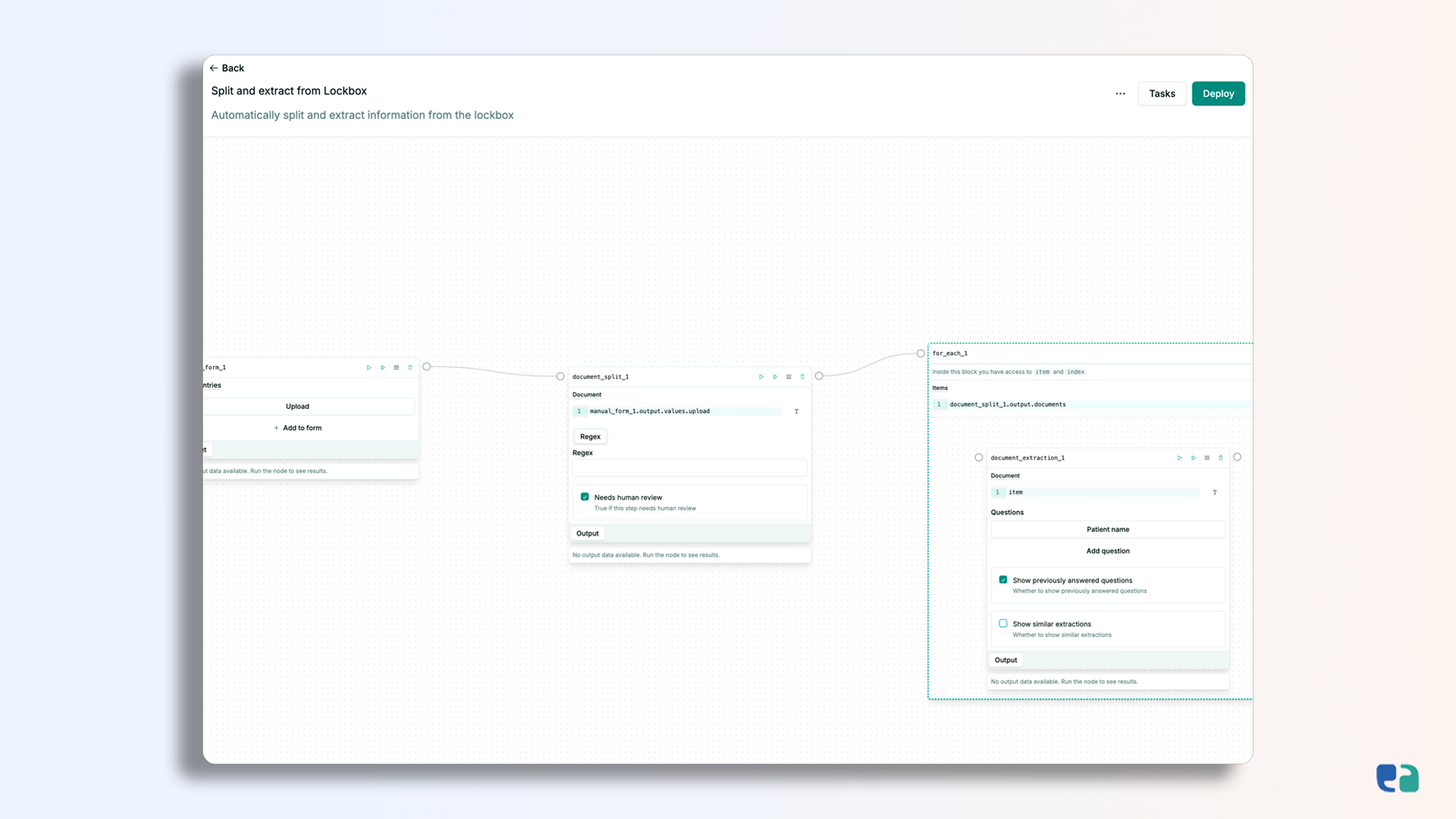
How We Developed an AI-Driven Solution to Redefine Healthcare Billing & Reimbursement
Technologies Powering Automated Medical Billing Solutions
To create top-notch automated billing solutions, we leverage cutting-edge technologies that ensure high performance, flexibility, and scalability. Here’s how we do it:
Custom vs. Pre-Built Medical Billing Software: What’s the Better Choice?
Choosing between custom and pre-built medical billing automation software is a big decision. Here’s why custom solutions often come out on top: