Let’s talk about Pharmacy Benefit Management (PBM) software.
It’s really shaking things up for healthcare organizations.
This software is a game changer for managing prescription costs and boosting patient care.
Think about it: with all the automation, it really simplifies things.
Healthcare providers can make smarter choices, keep track of drug lists more easily, and really help patients stick to their medications.
But don’t just take my word for it—check out these real-world examples:
- Blue Cross Blue Shield saved 15% on drug costs by using a PBM tool from Cerner.
- CVS Health made things easier for patients by using Express Scripts’ PBM to automate claims.
- Pfizer worked with MedImpact to track how well patients took their meds and made better treatments.
These examples show how PBM software can make a big difference in healthcare.
In this blog, we’ll talk about the important parts of PBM software, cool new tech, and how to design it to help you work better, save money, and make patients healthier.
What is PBM Software?
A specialized type of software designed to streamline the processes involved in managing prescription drug benefits.
It acts as a central hub for various stakeholders in the healthcare system, including:
- Pharmacies
- Health insurance companies
- Pharmaceutical manufacturers
- Patients
Common Problems Faced by PBM Companies in 2024 and How Software Can Help
PBM companies often encounter various challenges that can impact their efficiency, profitability, and member satisfaction.
Here are some common problems and how software solutions can address them:
Can Software Solve PBM Financial Model Issues?
Absolutely! Software can effectively address foundational problems in Pharmacy Benefit Management (PBM) financial models in several ways:
- Accurate Data Integration: Integrates real-time data on acquisition costs, rebates, and fees, eliminating reliance on outdated indices like AWP and ASP.
- Dynamic Pricing Models: Utilizes algorithms to reflect current market conditions, ensuring pricing is based on actual costs.
- Transparency and Reporting: Provides clear insights into PBM pricing, helping organizations assess the true financial value of contracts.
- Contract Management: Facilitates negotiations with standardized terms for true net acquisition costs, supporting better contract alignment.
- Accountability and Auditing: Automates audit trails and compliance checks, ensuring PBMs are held accountable for their pricing and rebates.
- Cost Modeling: Converts pricing into per member per month costs for accurate financial forecasting and accrual building.
Must-Have Features of Effective PBM Software
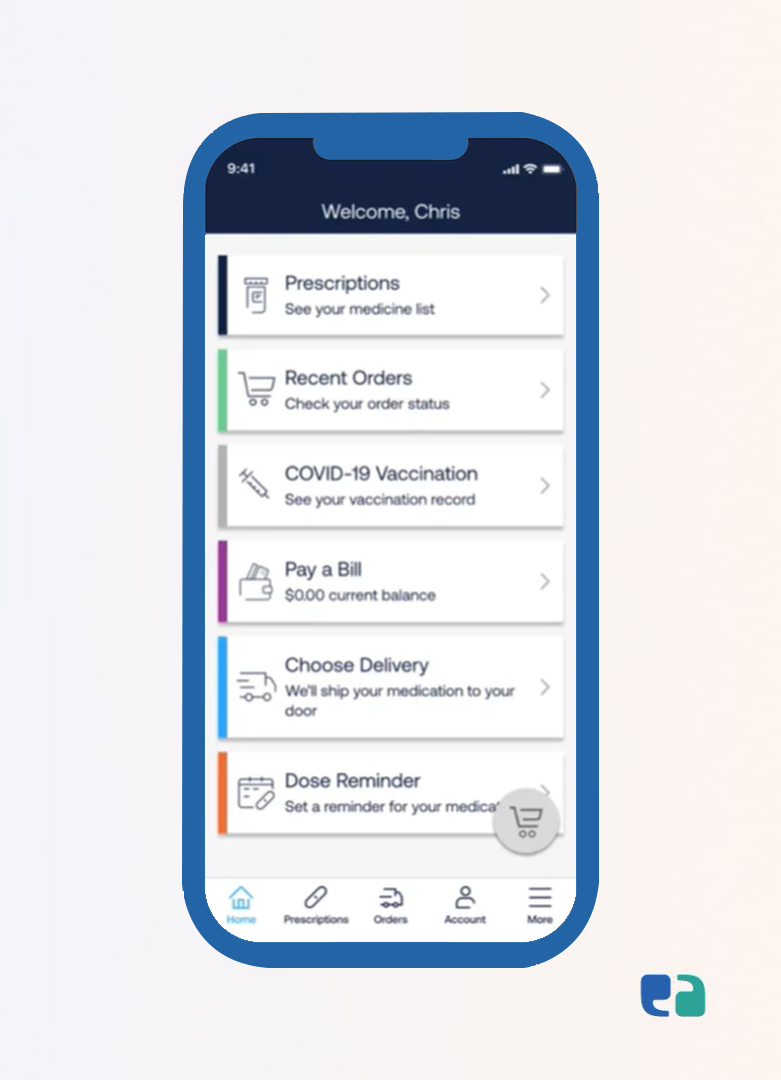
To optimize drug costs and improve patient care, effective PBM software is a must. Here are the key features to look for:
Top Pharmacy Benefit Management (PBM) Software

The PBM software market is competitive, with various providers offering different features and capabilities.
Here are some of the leading PBM software solutions:
5 Steps to Build Effective PBM Software
Building great Pharmacy Benefit Management (PBM) software takes more than just tech—it’s about solving real problems. Here’s how to do it:
1. Understand User Needs
Talk to healthcare professionals and patients.
Understand their pain points and design a solution that truly improves their day-to-day tasks.
2. Plan for Growth
Build software that can evolve.
Think ahead to ensure it can handle future demands, new features, and more users.
3. Keep it User-Friendly
Make the interface simple and easy to navigate.
Healthcare staff and patients should find it intuitive without a steep learning curve.
4. Ensure Smooth Integration
Your software must work seamlessly with existing systems like EHRs and pharmacy platforms. Integration is key for smooth operations.
5. Focus on Compliance
Healthcare regulations like HIPAA are non-negotiable.
Ensure the software meets all legal and privacy standards to keep patient data secure.
Why Partner with a Healthcare IT Expert
Developing PBM software can get complex, but a healthcare IT expert can simplify the process.
These professionals understand healthcare systems inside and out, ensuring your software meets all compliance standards from the start.
They also design solutions that can scale with your business and adapt to future needs.
Plus, they customize the software to fit your unique workflows, making it efficient and user-friendly.
With a trusted health-tech partner, you get more than just software—you get a solution built for the real-world challenges of healthcare.