Behavioral healthcare is facing some serious challenges.
While awareness of mental health issues is on the rise, the system is struggling to meet the growing demand.
Patients often face long wait times and limited access to specialized care.
A big part of the problem? Insurance billing and eligibility verification.
Providers spend too much time on administrative tasks, and most tools for verifying patient eligibility aren’t up to the mark—especially in behavioral health.
In fact, traditional eligibility checkers only hit about 50-60% accuracy in mental health services, mainly because they don’t account for payer carve-outs, where insurers outsource behavioral health coverage to third-party providers.
This inaccuracy leads to frequent insurance claim denials—impacting 11% of patients seeking behavioral health care.
For providers, these denials result in revenue losses, higher employee workloads, and inflated marketing costs.
To tackle this, building a more reliable patient eligibility verification tool can drastically reduce claim denials and streamline the administrative process.
By solving these inefficiencies, providers can focus more on patient care and less on paperwork.
The High Cost of Inaccurate Claims in Behavioral Health
Denied insurance claims in behavioral health create huge financial problems for both providers and patients.
Unfortunately, up to 11% of patients face claim denials, leading to revenue loss for providers and making it harder for patients to access care.
A major reason behind these denials? Preventable errors in eligibility verification and medical coding.
In fact, 85% of these denials are avoidable, amounting to a staggering $40 billion in preventable losses.
These errors happen early in the revenue cycle, during eligibility verification and coding, where manual processes and outdated tools lead to costly mistakes.
For providers, this means reduced revenue, increased staff workload, and strained budgets.
The Challenges of Eligibility Verification
Insurance eligibility verification is tricky, especially in behavioral health.
A big issue is payer carve-outs, where insurance companies hand off certain services, like behavioral health, to third-party insurers.
This creates confusion and makes it difficult for providers to figure out which payer is responsible for coverage.
Traditional automated tools used for eligibility checks aren’t equipped to handle these complexities.
They often miss payer carve-outs, leading to only 50-60% accuracy in verifying coverage for mental health services. This inaccuracy results in:
- Incorrect Benefits Info: Providers might tell patients the wrong details about their coverage.
- Out-of-Network Billing: Missing a carve-out can result in billing the wrong insurer, leading to higher costs for patients.
- Frequent Claim Denials: Claims submitted to the wrong payer often get denied, causing delays and financial losses.
These preventable errors place a heavy burden on providers and disrupt patient care.
To avoid these issues, behavioral health providers need better tools to accurately verify patient eligibility and reduce costly denials.
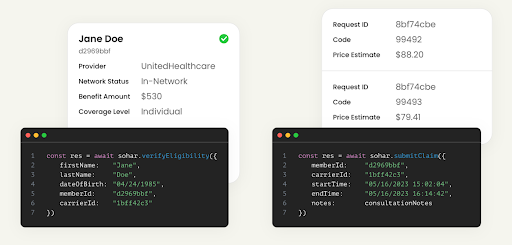
Introducing Sohar Health: A Solution for Behavioral Health RCM
Sohar Health is making a big difference in solving the challenges of inaccurate claims and manual processes in behavioral health.
This San Francisco-based startup was founded in 2023 by Dr. Ashish Mandavia and Lucas Gordon.
They created a SaaS platform that helps behavioral health providers streamline and improve their revenue cycle management (RCM).
Sohar Health’s solution is designed specifically to make the billing process smoother and more accurate for providers, reducing errors and saving time.
Sohar Health’s Impact: Boosting Efficiency, Revenue, and Patient Care
Sohar Health’s solution combines accurate eligibility checks with AI-powered medical coding.
This makes a big difference for behavioral health providers and improves patient care in several ways:
1. Increased Revenue
Sohar Health helps providers recover lost revenue.
By reducing claim denials and ensuring correct reimbursements, providers can get back up to 20% of what they lost.
2. Enhanced Efficiency
Automating eligibility checks and medical coding cuts down the administrative work for providers.
This saves time and resources that can be focused on patient care. It also reduces manual data entry, leading to fewer mistakes and better operations.
3. Improved Patient Experience
With accurate eligibility info available, providers can give patients clear details about their coverage and costs upfront.
This transparency builds trust, lessens billing surprises, and makes patients happier.
4. Focus on Patient Care
By easing the administrative load of revenue cycle management, Sohar Health allows providers to spend more time on what really matters: delivering high-quality care that centers around the patient.
Founders:
Ashish & Lucas
3 Takeaways for Building a Solution Like Sohar Health
If you’re thinking about creating a solution similar to Sohar Health, especially in the behavioral health tech space, there are some valuable lessons to consider. Here are key takeaways that can guide you on your journey:
Building Your Solution: 3 Key Features to Consider
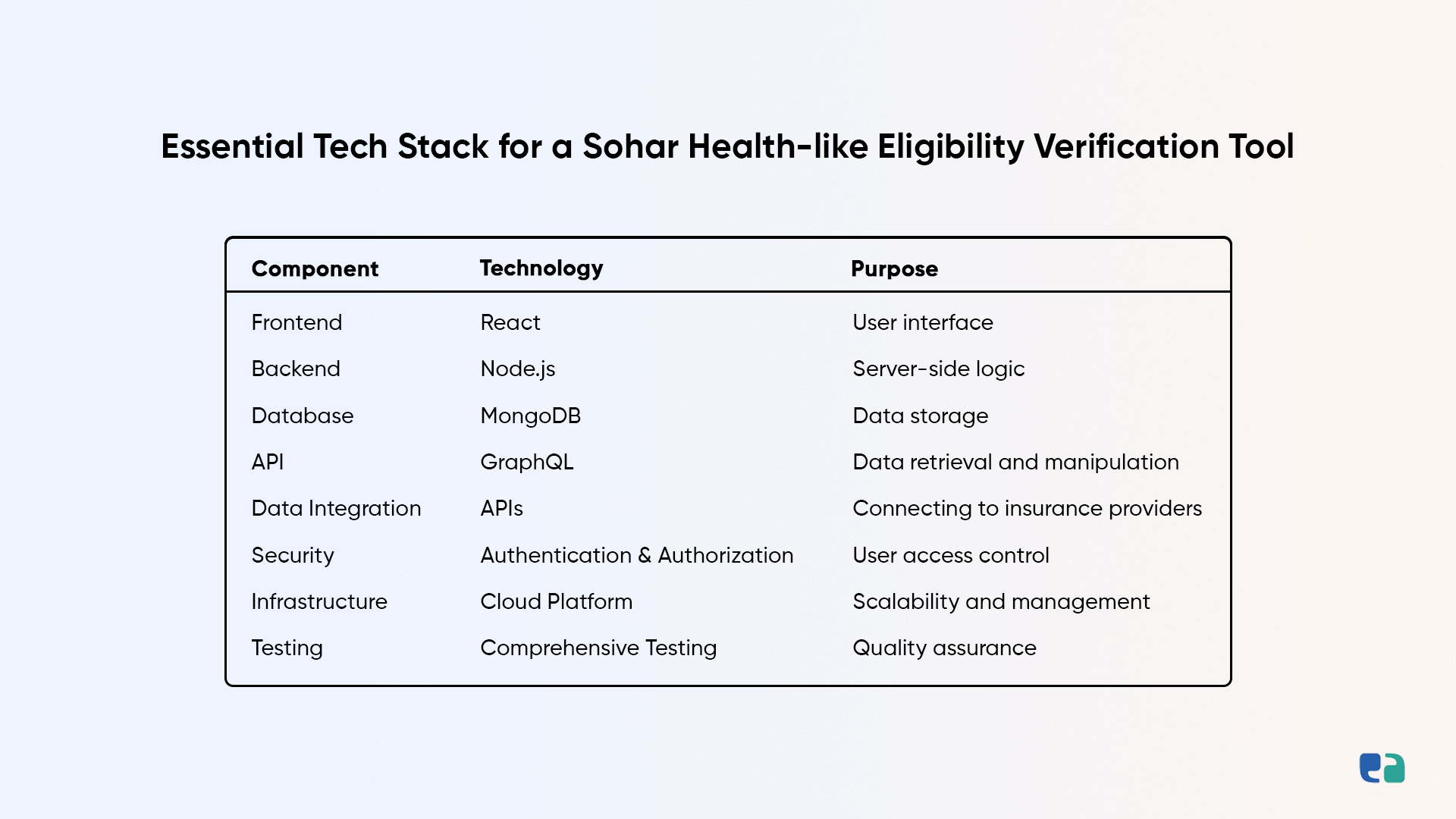
4 Steps to Build A Successful Patient Eligibility Verification Solution
This section outlines a step-by-step guide for entrepreneurs looking to build a successful Patient Eligibility Verification solution, using Sohar Health as a prime example.
Limitations of Sohar Health & An Alternative Solution
Sohar Health is a useful tool for behavioral health providers, but it has some limitations.
Being cloud-based, it relies on stable internet, and any disruptions can affect real-time eligibility checks.
It also doesn’t integrate with all payer systems, which can lead to gaps in patient verification.
The setup process can be time-consuming and requires technical expertise, posing challenges for organizations with limited resources.
Additionally, accuracy can vary based on the payer, so providers may need to double-check eligibility data.
Given these issues, custom solutions may be preferable.
They offer greater flexibility in integration, enhance user experience with tailored interfaces, improve data accuracy, and streamline.