Ever wondered how you could simplify the complicated process of payment collection in your healthcare practice?
You’re not alone. Payment collection in healthcare is tough.
Providers deal with multiple payers, each with its own system.
Plus, payor systems rarely communicate with provider EMRs, leaving a lot of manual work that costs both time and money.
In fact, healthcare providers spend a staggering $300 billion a year just to get paid, and even then, many collect less than they’re owed.
For skilled nursing facilities (SNFs), this situation is even worse.
With increasing costs and complicated reimbursement processes, many SNFs face critical financial challenges, often losing money due to missed payments or denied claims.
But here’s the good news—CoreCare’s clinical reimbursement solution is here to change that.
By securing faster payments and reducing write-offs, it helps SNFs improve cash flow and focus on what they do best: delivering top-quality care.
CoreCare: Simplifying Billing and Payment Collection for Healthcare Providers
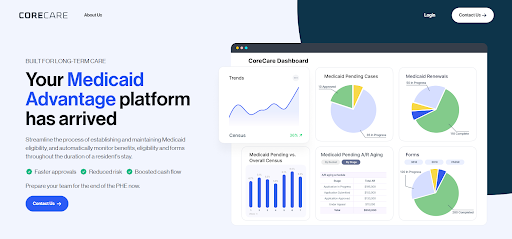
CoreCare, a leading provider of revenue management services, helps healthcare companies streamline their billing and payment processes.
Using machine learning, CoreCare automates billing, paperwork, and revenue cycle management, significantly reducing administrative burdens for hospitals and skilled nursing facilities (SNFs).
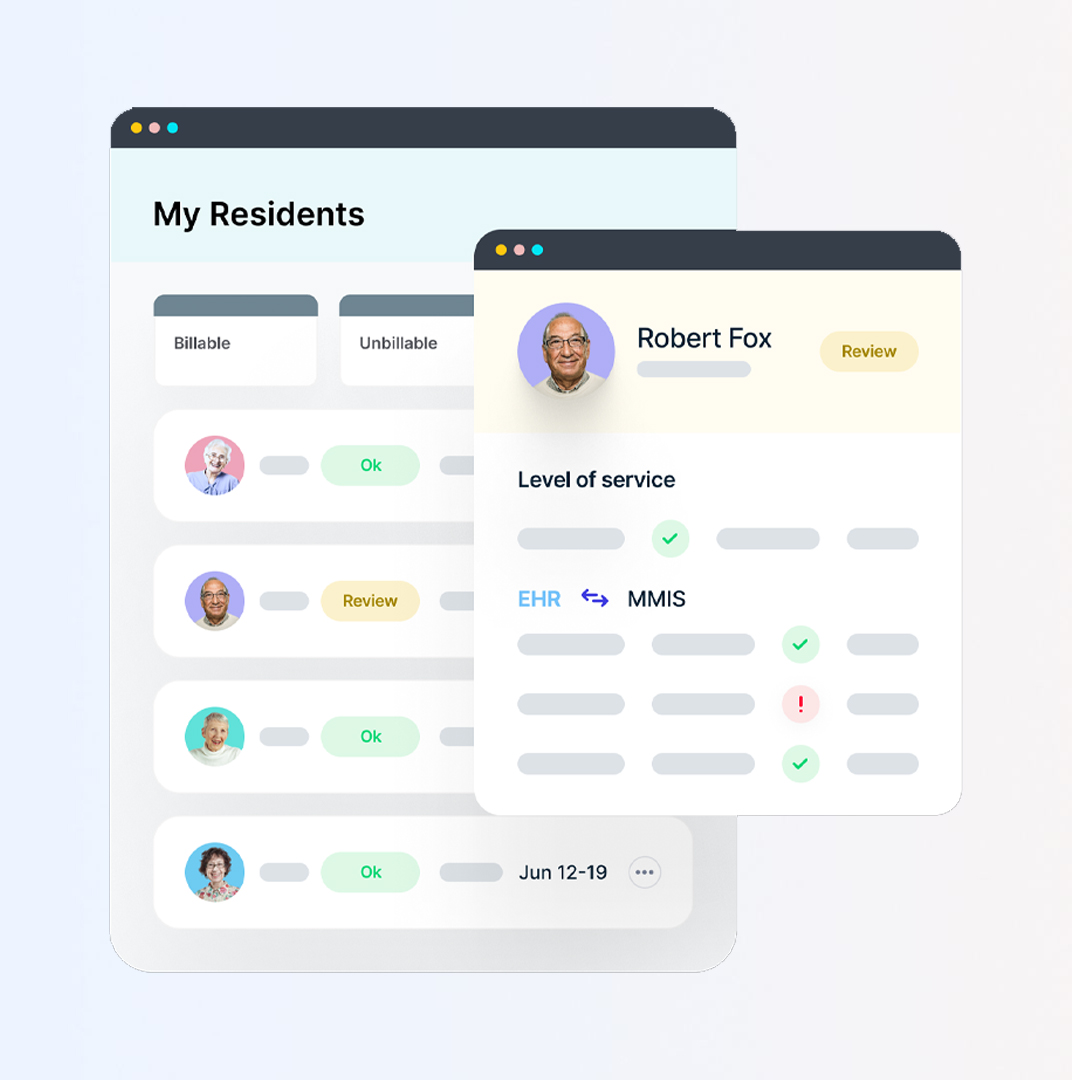
By linking electronic health records (EHRs), Medicare, Medicaid, and payer systems, CoreCare creates a single, unified view of patient data.
This allows healthcare providers to automate workflows and eliminate manual tasks, resulting in fewer payment delays and reduced costs.
With a subscription model ranging from $300 to $500 per facility, CoreCare is transforming how healthcare providers manage their revenue.
“We’re proud to be one of CoreCare’s first partners in Ohio,” said John Renner, CFO of United Church Homes. “We heard how SNFs were using CoreCare to automate eligibility workflows, and we knew we had to bring that level of innovation into our organization. Our facilities, regional and corporate staff now have a powerful platform that simplifies our operations, improves our cashflow, and increases our revenue.”
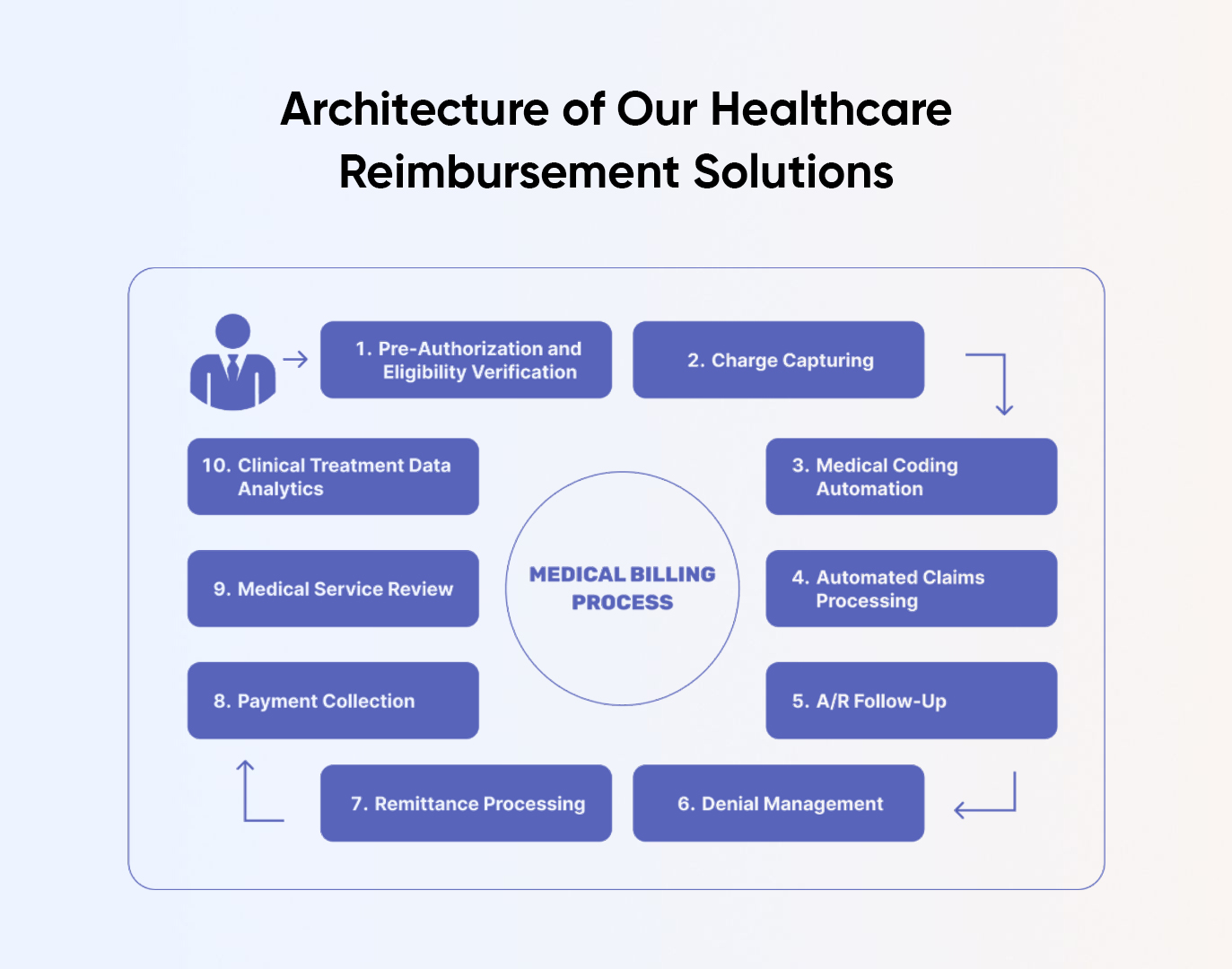
CoreCare’s Solution: A Model for Payment Collection
CoreCare is an example of how to simplify the payment collection process in healthcare. Their solution is designed to make things easier for providers. Here’s how they do it:
By examining CoreCare’s approach, healthcare providers can find inspiration to develop their own solutions for streamlining payment collection and enhancing revenue management.
Clinical Reimbursement Solution: The Success Behind CoreCare
At the heart of CoreCare’s success is its robust healthcare reimbursement solution.
This solution addresses one of the most challenging aspects of healthcare management—getting paid.
By streamlining the reimbursement process, CoreCare helps healthcare providers minimize claim denials, reduce administrative costs, and get paid faster.
With intelligent automation, CoreCare eliminates much of the manual work involved in claim processing, ensuring accuracy and speed.
Their real-time analytics offer valuable insights that allow providers to identify and fix potential issues before they become costly problems.
Additionally, their patient-friendly billing options enhance the overall patient experience while improving cash flow.
This focus on efficient, tech-driven reimbursement management has made CoreCare a trusted partner for healthcare providers looking to optimize their revenue cycles and reduce financial stress.
It’s clear that their success is rooted in their ability to simplify and enhance the entire reimbursement process.
Features of Clinical Reimbursement Solutions
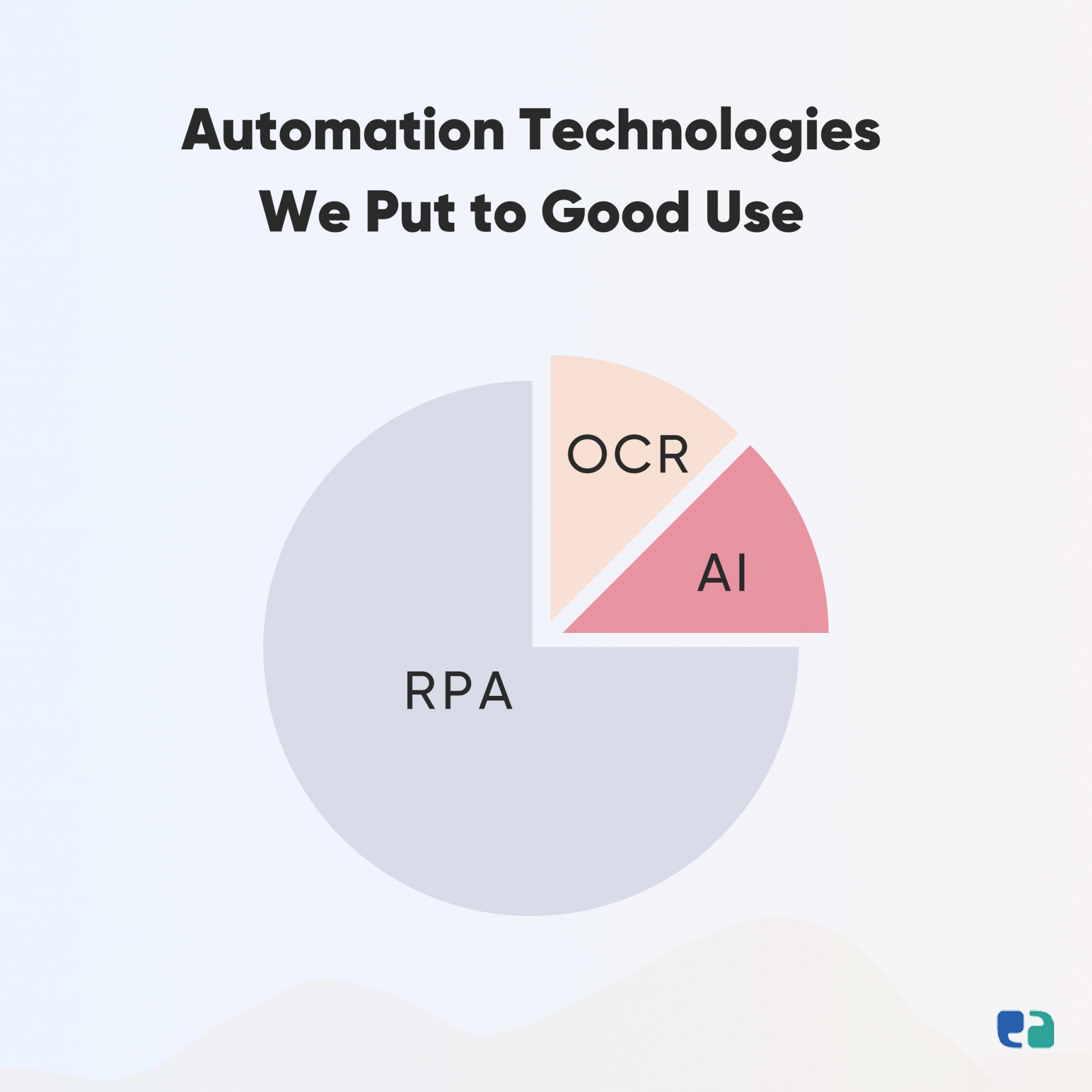
Technologies Powering Automated Clinical Reimbursement Solutions
When it comes to automated clinical reimbursement solutions, leveraging cutting-edge technologies is key to ensuring high performance, flexibility, and scalability.
Here’s a look at some of the essential technologies making a difference:
Want to Build a Clinic Reimbursement Solution? You Have Two Options!
When considering a clinic reimbursement solution, you typically have two paths: custom solutions and SaaS (Software as a Service) solutions.
While CoreCare offers a SaaS option, building a custom solution could be the smarter choice for several reasons.
In summary, while SaaS solutions like CoreCare’s may offer quick deployment, investing in a custom clinic reimbursement solution can provide the flexibility and long-term value that your healthcare practice truly needs. You can also calculate the software cost for custom, white-label and SaaS platform.