Healthcare is a complex field.
It’s crucial that medical billing runs efficiently to make sure healthcare providers are fairly compensated for their services.
However, one element of medical billing that’s often overlooked but equally important is credentialing.
In this blog, we’ll delve into the intricacies of credentialing in medical billing, uncovering common mistakes that can happen during this process, and exploring how automated credentialing can be a game-changer for the healthcare industry.
Get ready to discover how credentialing can help streamline the medical billing process and ensure that healthcare providers get the compensation they deserve!
Understanding Credentialing in Medical Billing
Are you familiar with the term ‘credentialing’?
It’s a meticulous process ensuring healthcare providers meet the high standards of insurance companies and other healthcare organizations.
This process helps establish trust, quality, and compliance in healthcare services, which is crucial for patients to receive the best care possible.
Without proper credentialing, healthcare providers may face challenges in receiving reimbursements for their services.
It’s an important aspect of the healthcare industry that ensures patients receive quality care from qualified providers.
Common Mistakes in Medical Billing Credentialing
Mistakes in the credentialing process can lead to a cascade of issues, including reimbursement delays and potential legal troubles.
It’s crucial to be aware of these common pitfalls to avoid them:
Automated Credentialing in Medical Billing
Are you tired of dealing with the countless errors and delays in the credentialing process that often lead to revenue loss?
Well, it’s time to say goodbye to those worries!
Many healthcare organizations have found a solution to these problems by adopting automated credentialing systems.
Trust us, the benefits of using automated credentialing in medical billing are simply outstanding.
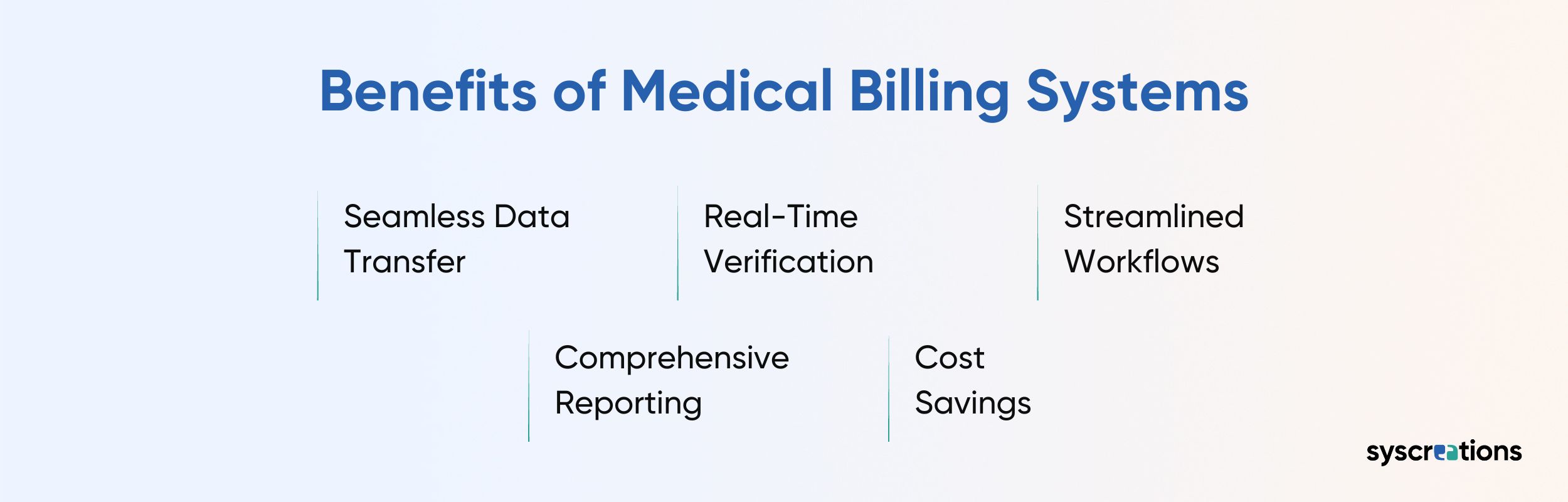
Credentialing Medical Software and Integrated Medical Billing Systems
As technology continues to advance, the healthcare industry has witnessed a proliferation of credentialing medical software and integrated medical billing systems.
These software solutions not only automate the credentialing process but also seamlessly integrate it with medical billing operations.
The benefits of such software are multifaceted:
Streamline Your Medical Billing with Software
The world of medical billing can be a confusing maze.
The importance of the credentialing process often gets noticed once problems arise.
But what if there was a way to make the process smoother, more efficient, and less prone to errors?
Well, there is!
It’s through the power of automation and integrated software solutions!
By adopting these technological advancements, healthcare providers can reduce mistakes, improve financial reimbursement, and deliver high-quality care to patients.
So, let’s embrace automation and unlock the full potential of credentialing, making healthcare better for everyone!